As we continue to raise awareness for American Heart Month, we’re providing some brief introductions to heart health and disease. Heart disease remains the No. 1 cause of death in the United States since 1950. These are by no means exhaustive, and we encourage you to speak with your provider about your own heart’s health and any concerns you may have. With that, let’s briefly touch on Atrial Fibrillation (AFib)..
What is Atrial Fibrillation (AFib)? This condition has to do with rapid, irregular heartbeats – also known as a type of arrhythmias – in the heart’s upper chambers. These upper chambers, or atria, then aren’t pumping blood efficiently and regularly to the lower chambers, or ventricles. With AFib, they’re quivering, sending wildly irregular electrical signals. You could say that, from this, the entire heart gets all out of sorts. With irregular, fast, uncoordinated rhythms and thus inefficient, irregular blood flow to the ventricles, clots can form and in turn increase the risk of stroke.
Symptoms? Symptoms include heart palpitations, dizziness/lightheadedness, chest pain and/or discomfort, shortness of breath, fatigue, and weakness.
Are there different types? There are actually four types:
Paroxysmal – Very brief episodes with spontaneous starts and stops; with this type, it’s usually within 7 days, if not within 24-48 hours.
Persistent – Longer than 7 days and will often require medical intervention to get the heart back into normal rhythm. These interventions may include electrical cardioversion or medication.
Long-standing Persistent – Lasts for more than 12 months.
Permanent – The arrhythmia is long-term and constant. A patient and provider may decide to abort interventions intended to normalize the heart’s rhythm and instead put their focus on rate control.
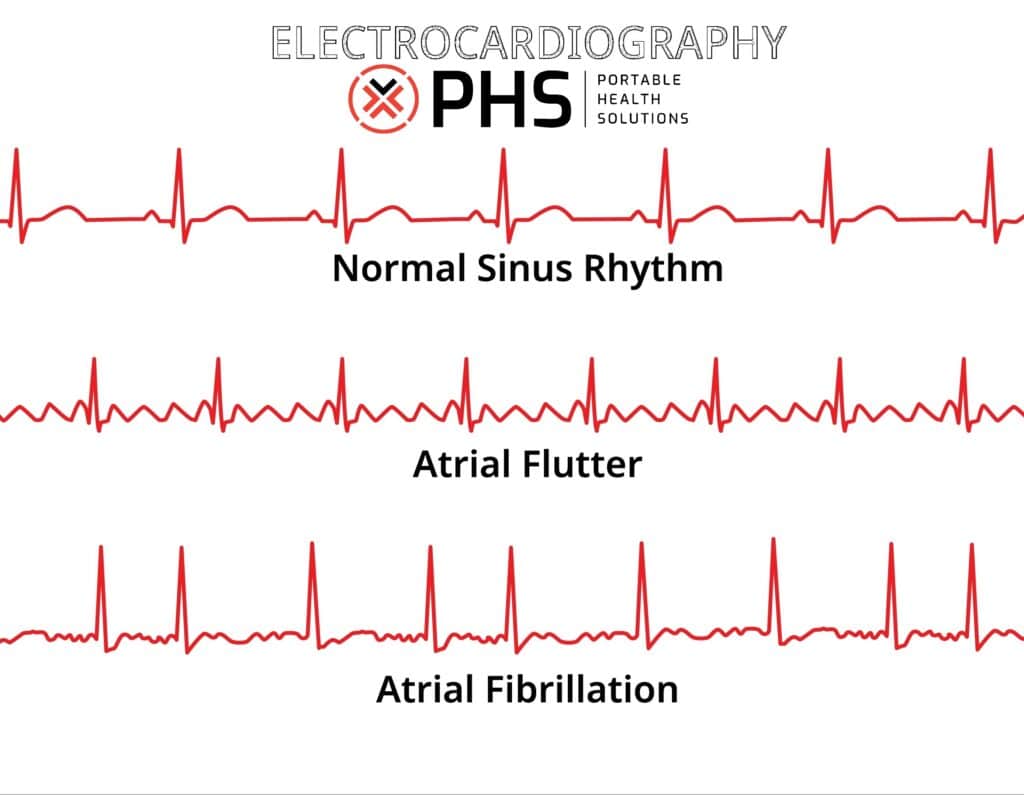
Diagnosis? There are many options, starting with the primary tool: Electrocardiogram, or EKG, which PHS offers as a service! This records electrical signals that can confirm if there is arrhythmia.
Others include:
Holter Monitor – Portable device to record heart activity during a patient’s daily routines; usually 24-48 hour recordings.
Loop Recorder (implantable) – Continuous with a device placed just under the skin; as you might imagine, this is for long-term monitoring of up to three years.
Event recorder – Designed to catch infrequent symptoms, this can be used for weeks to months.
Echocardiogram – Another offering by PHS, this is a heart ultrasound to check for blood clots, valve issues, or structural problems.
Blood tests – One wouldn’t automatically think of a blood test as being an option, but with this, thyroid function and electrolyte imbalance can be evaluated, as well possible infection. Any of these could trigger AFib.
Stress test – The monitoring of heart rhythm during physical exercise.
Wearable tech – Some smartwatches and similar devices that can detect heart rate and rhythm, building data for a provider.
Why is AFib a thing? The body and its environment is nothing if not complex. AFib can be caused by structural damage to heart tissue stemming from heart disease, aging, high blood pressure, hypertension, obstructive sleep apnea, genetics, hyperthyroidism, diabetes, neurologic disorders, alcohol consumption, and many more.
Would you like to learn more? Here are some outstanding resources for learning about this condition: